Does The Menopause Affect Your Pelvic Floor?
The simple answer is, yes - the menopause can affect your pelvic floor. Beyond the well-known symptoms like hot flashes and mood swings, menopause brings about changes in the body that can impact various aspects of health, including the pelvic floor.
In this blog post, we will explore how menopause affects the pelvic floor muscles and discuss proactive ways to address pelvic health during this significant life stage.
How Menopause Affects the Pelvic Floor Muscles
1. Tissue Atrophy
During menopause, estrogen levels decline, impacting the thickness and elasticity of vaginal and urethral tissues. Estrogen plays a crucial role in maintaining the health of these tissues, and its decrease can lead to tissue atrophy. This can result in discomfort, dryness, and an increased susceptibility to infections.
Unfortunately too many women suffer in silence with this assuming that it is 'just' a factor of getting older. Please do see your medical practitioner and for most women this can be treated relatively quickly with estrogen.
Topical vaginal estrogen effectively addresses symptoms of vaginal atrophy without elevating systemic estrogen levels. This treatment is accessible in various forms, including cream, vaginal pills, and rings. Your healthcare provider can guide you through each option, helping you determine the most suitable choice based on your individual needs.
For a deeper understanding of how estrogen influences the pelvic floor, check out our blog on How Estrogen Can Affect Your Pelvic Floor.
2. Urinary Incontinence & Frequency
Weakened pelvic floor muscles may struggle to adequately support the bladder and urethra, leading to urinary incontinence and increased frequency. The loss of muscle tone can make it challenging to control the release of urine, impacting a woman's daily life and causing embarrassment. Understanding these changes is crucial during the menopause.
3. Pelvic Organ Prolapse
The decreased estrogen levels during menopause can contribute to weakened pelvic floor support, potentially resulting in pelvic organ prolapse. This condition occurs when the pelvic organs, such as the bladder or uterus, descend into the vaginal space. It can lead to discomfort, a feeling of fullness, and even impact sexual function.
4. Sexual Dysfunction
Menopause can bring about changes in sexual function due to hormonal shifts and the effects on pelvic floor muscles.
Vaginal dryness, decreased libido, and discomfort during intercourse are common concerns. Understanding these issues is crucial for seeking appropriate solutions to maintain a fulfilling sex life during and after menopause.
5. Changes in Connective Tissues
Menopause can lead to alterations in connective tissues within the pelvic region. Estrogen, which is essential for maintaining the strength and flexibility of connective tissues, diminishes during menopause. This reduction can result in weakened support for pelvic organs, contributing to issues like pelvic floor dysfunction.
Understanding the role of connective tissues in pelvic health provides valuable insights into the broader implications of menopause on the body.
6. Impact on Muscular Coordination
Menopause not only affects muscle tone but can also impact muscular coordination within the pelvic floor. The intricate interplay of muscles in this region is essential for various functions, including bladder and bowel control.
Hormonal changes during menopause may disrupt this coordination, leading to issues like fecal incontinence or difficulty controlling bowel movements.
Understanding these complexities can empower women to seek targeted interventions and exercises for improving muscular coordination.
7. Psychological Impact on Pelvic Health
The hormonal fluctuations and physical changes during menopause can also have a psychological impact on pelvic health. Issues such as anxiety, depression, or stress can contribute to pelvic floor dysfunction.
Recognizing the interconnectedness of mental health and pelvic well-being is crucial for a holistic approach to managing menopausal symptoms.
Incorporating stress-reduction techniques and seeking emotional support can be integral components of maintaining optimal pelvic health during this life stage.
"Self Care Isn't Selfish"
How to Proactively Address Pelvic Health in Menopause
To proactively address pelvic health during menopause, women can incorporate targeted exercises, known as 'Kegels' into their daily routines. You should be aiming for 2 to 3 sets a day - EVERY Day!
To ensure that you are doing your Kegels correctly and for best results, you can use our pelvic floor toner:
Secret Whispers Pelvic Floor Toner is designed to strengthen your pelvic floor muscles in a safe and effective way to help improve bladder control, enhance sexual sensation, and promote overall pelvic health. Just 15 minutes a day is all that is needed.
Additionally, vaginal estrogen therapy may be recommended to counteract the effects of declining estrogen levels. These approaches aim to strengthen and maintain the health of pelvic floor muscles.
In conclusion, understanding the multifaceted impact of menopause on the pelvic floor is crucial for women's overall well-being. By addressing various aspects, from tissue health to psychological well-being, women can navigate this life stage with resilience and proactive strategies.
For more information on menopause, pelvic prolapse and related topics, check out our blog.
- 27 Pages full of lots of great information.
- Recommended foods you can eat to help you naturally increase your estrogen and some fabulous recipes.
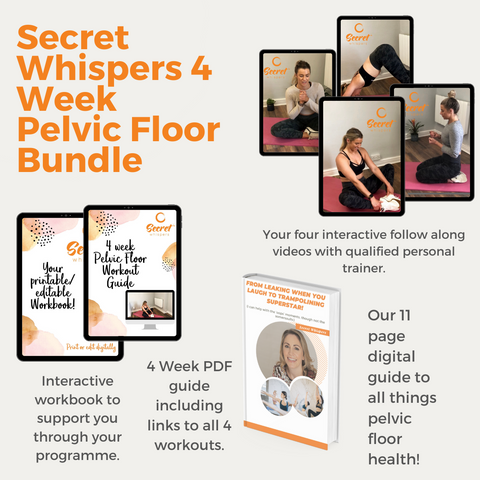
YOUR 4 WEEK PELVIC FLOOR MUSCLES WORKOUT PROGRAMME
Designed to be done anywhere and at any time. Yours to keep forever.